If you’re wondering, “What does shoulder arthritis feel like?” imagine a deep ache or sudden sharp pain in your shoulder that stays with you, reducing your range of motion and making everyday tasks difficult.
In this post, I’ll dive into the symptoms of shoulder arthritis, and try to help you understand why these sensations occur, promising insight into managing the condition without diving too deep into treatment solutions.
Key Takeaways
- Shoulder arthritis is characterized by symptoms such as persistent pain, stiffness, limited range of motion, and can impact sleep and everyday activities, with symptom severity varying among different types of arthritis (osteoarthritis, rheumatoid arthritis, post-traumatic arthritis).
- Diagnosis of shoulder arthritis typically involves a review of medical history, physical examinations, and imaging tests like X-rays, MRI, and ultrasound to assess the extent of the condition and tailor an appropriate treatment plan.
- Treatment options for shoulder arthritis range from non-surgical methods such as lifestyle modifications, physical therapy, and medications to surgical procedures like arthroscopic debridement and shoulder joint replacement, depending on severity and individual patient needs.
Experiencing Shoulder Arthritis: How It Feels
Shoulder arthritis weaves itself into the fabric of everyday life, presenting symptoms that extend beyond the occasional joint pain. Those living with shoulder arthritis often describe a persistent discomfort that doesn’t relent with rest and can significantly disrupt sleep. The pain may not always be linked to the arm’s movement but can radiate, creating a path of discomfort from the shoulder down to the elbow and wrist in more severe cases.
It’s a condition that creates a range from mild to severe pain and stiffness, curtailing the shoulder’s range of motion and impacting the quality of life.
Pain and Stiffness in the Shoulder Joint
The pain associated with shoulder arthritis can manifest as a deep, penetrating ache or a sharp, sudden discomfort within the joint, often intensifying during activity or motion. This pain is not a mere inconvenience; it’s a reminder of the degenerative nature of the condition, particularly if the glenohumeral joint is affected. Stiffness and swelling join forces, further contributing to a diminished range of motion that can make even simple tasks like lifting the arm an ordeal.
The weather itself can become an adversary, with changes often bringing about an increase in pain, especially for those with shoulder osteoarthritis.
Impact on Daily Activities
Shoulder arthritis stealthily invades daily routines, transforming mundane activities into feats of endurance. It’s not just the sharp jabs of pain while reaching for a high shelf; it’s the deep ache that follows simple actions like bathing, grooming, or even writing. Everyday tasks that require shoulder motion, including those involving the shoulder blade, can become sources of discomfort, and the joint pain can impede participation in sports and activities once enjoyed without a second thought.
The condition forces individuals to navigate their day with a heightened awareness of their limitations, seeking ways to perform tasks without provoking the wrath of their own joints.
Types of Shoulder Arthritis and Their Symptoms
Shoulder arthritis is not a one-size-fits-all condition; it manifests in various forms, each with its symphony of symptoms. The common thread among them includes joint sounds like grinding or popping, tenderness around the shoulder area, and a noticeable loss of range of motion.
From the symmetrical pain of rheumatoid arthritis to the injury-induced post-traumatic arthritis, each type brings its unique challenges. It’s crucial to understand the distinct characteristics of these variants, as they directly influence the approach to treatment and management.
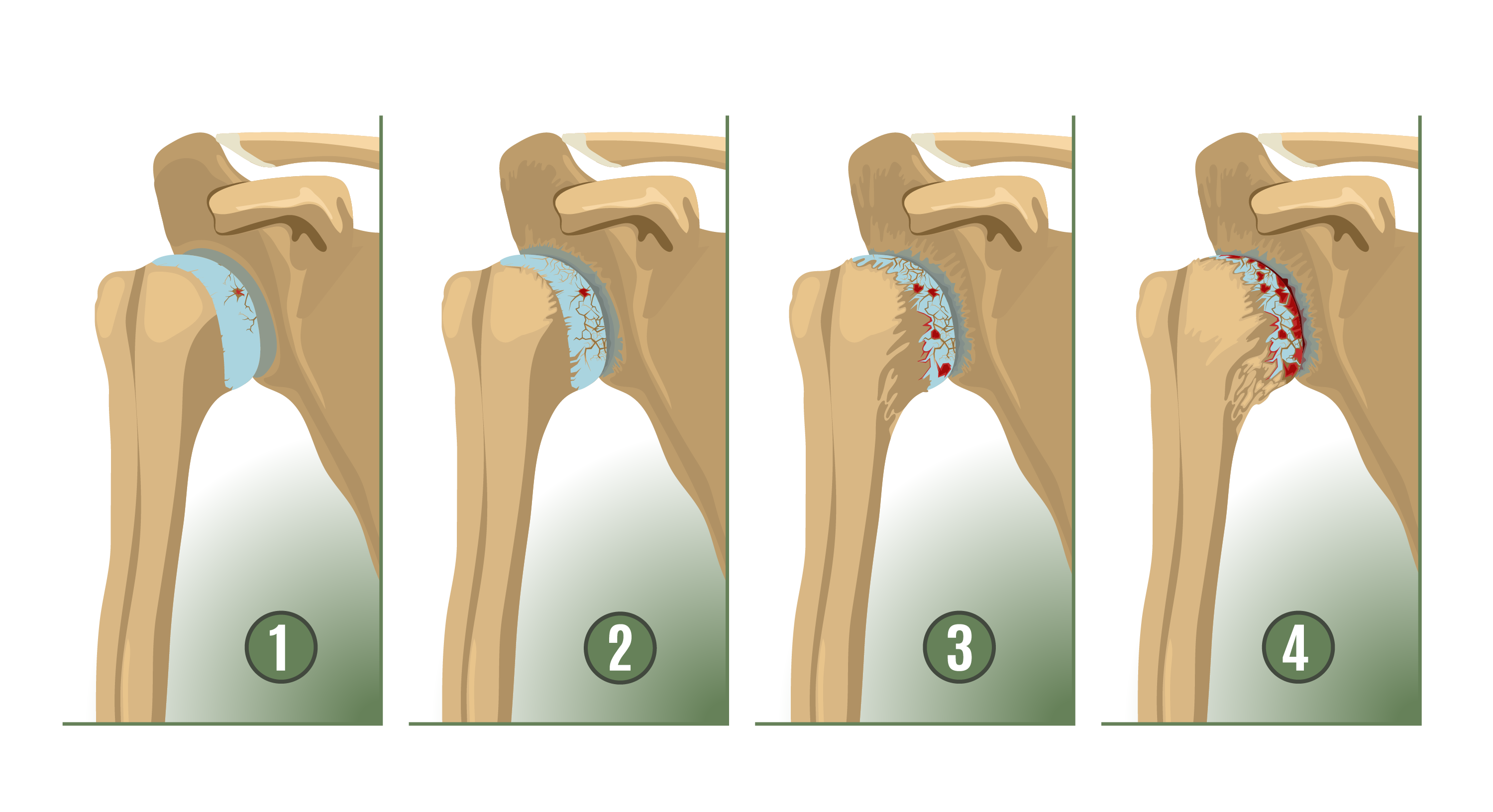
Osteoarthritis
Osteoarthritis, often dubbed the ‘wear and tear’ arthritis, typically targets those over 50, leaving its mark on the acromioclavicular joint, which connects the arm bone to the shoulder blade. Pain in the side or back of the shoulder is a telltale sign, along with a tendency to worsen with activity or shifts in the weather.
This degenerative joint disease slowly erodes the shoulder’s cartilage, leading to an escalation of discomfort during activities that place stress on the joint, like lifting or carrying heavy objects. The prevalence of shoulder osteoarthritis serves as a reminder of the joint’s vulnerability to the relentless march of time.
Rheumatoid Arthritis
Rheumatoid arthritis, an autoimmune disease, wreaks havoc symmetrically, often affecting both shoulder joints with a vengeance. The disease’s hallmark is a swollen synovial lining within the joints, which triggers pain and stiffness that can profoundly alter one’s daily life. With rheumatoid arthritis, the immune system mistakenly attacks the body’s tissues, leading to chronic symptoms that demand a vigilant treatment plan.
The widespread impact of this inflammatory arthritis underscores the importance of early detection and comprehensive management.
Post-Traumatic Arthritis
In the aftermath of a shoulder injury, post-traumatic arthritis looms as a potential consequence, bringing persistent pain and stiffness that can evolve into chronic issues. This form of arthritis, more common in younger individuals, can curtail the ability to perform movements essential to daily life and recreational activities. It’s a condition that often stems from a history of shoulder dislocations or fractures, with symptoms that can increment over time.
For those with a severe form such as rotator cuff tear arthropathy, the weakness in the shoulder can be particularly pronounced.
Identifying Shoulder Arthritis: Diagnosis Process
To diagnose shoulder arthritis, a meticulous process is followed that begins with a comprehensive review of medical history and proceeds through a physical examination, supported by imaging tests that bring the interior landscape of the joint into sharp relief.
The diagnosis is critical to crafting a treatment plan that addresses the specific needs of the individual, paving the way for more targeted and effective interventions.
Medical History Review
A thorough dive into one’s medical history lays the groundwork for understanding the progression of shoulder arthritis. An experienced orthopedic surgeon will probe for insights into the onset and evolution of symptoms, the impact on daily activities, and any related health issues that might influence the condition. This step in the diagnosis process aims to unravel the severity and consistency of the discomfort experienced, as well as any patterns of stiffness or mobility loss that have emerged over time.
The medical history review is a critical phase in painting a complete picture of the patient’s condition and setting the stage for subsequent diagnostic steps.
Physical Examination
During the physical examination, the orthopedic shoulder surgeon becomes a detective, searching for clues within the shoulder’s movement and structure that point to arthritis. They inspect, palpate, and evaluate the shoulder’s range of motion, listening for any sounds that might indicate joint damage. This examination is not just about observing the present symptoms; it’s about distinguishing between osteoarthritis and other possible injuries.
Employing a systematic approach, the doctor assesses both passive and active range of motion and tests the shoulder’s strength, ensuring that no stone is left unturned in the quest for an accurate diagnosis.
Imaging Tests
The role of imaging tests in diagnosing shoulder arthritis cannot be overstated. Here are some of the key imaging tests used:
X-rays
- X-rays serve as the cornerstone, revealing the extent of cartilage damage and the presence of bone spurs.
MRI and Ultrasounds
- For a more nuanced look at the shoulder’s soft tissues, MRI and ultrasound are invaluable tools that can uncover conditions not visible on X-ray, such as tendon injuries.
Magnetic Resonance Arthrography
- Magnetic resonance arthrography, sometimes combined with a CT scan, provides a highly sensitive view of the complex structures within the shoulder, crucial for detecting lesions in the labrum and capsulo-ligamentous components.
These imaging tests are essential for accurately diagnosing shoulder arthritis and determining the appropriate treatment plan.
The choice between MRI and ultrasound often hinges on various factors, including the quality of imaging available and the expertise of the radiologist.
Non-Surgical Treatment Options for Shoulder Arthritis
When living with shoulder arthritis, non-surgical shoulder arthritis treatment options can be a beacon of hope, offering ways to manage symptoms and maintain joint health without going under the knife. Lifestyle modifications, physical therapy, and medications form the trinity of non-surgical interventions that cater to the nuances of each individual’s experience with the condition.
Lifestyle Modifications
Modifying one’s lifestyle is a proactive step in the battle against shoulder arthritis symptoms. Simple adjustments to daily activities, coupled with self-management strategies, can lead to significant pain alleviation. Relaxation and coping skills are essential in maintaining a positive mindset while managing the symptoms. The impact of weight management on symptom relief cannot be ignored, as excess weight can hasten joint degeneration.
Dietary changes, such as increasing the intake of fruits and vegetables and reducing processed foods, can also play a crucial role in symptom management. Employing joint protection techniques like pacing activities and using assistive devices can prevent additional joint stress.
Physical Therapy and Exercise
Physical therapy and exercise are pillars of non-surgical treatment, designed to fortify the muscles around the shoulder joint and enhance flexibility. Customized programs aim to restore range of motion over time, with a focus on strength training and flexibility exercises. Engaging in light to moderate physical activity is vital for protecting joints, as it strengthens supporting muscles and promotes circulation to the joint.
A gradual increase in exercise intensity is recommended, with a goal of 150 minutes of moderate-to-vigorous exercise weekly. Some low-impact exercises that can be particularly beneficial for maintaining mobility and managing symptoms include:
- Swimming
- Cycling
- Tai Chi
- Yoga
These exercises can help you stay active and improve your overall well-being.
Medications and Injections
Medications and injections play a critical role in the nonsurgical management of shoulder arthritis. Some options to consider are:
- Over-the-counter options like acetaminophen and NSAIDs, which are often the first line of defense against pain and inflammation. However, they must be used with caution due to the risk of liver damage and other side effects.
- Prescription anti-inflammatories, which may provide more relief for those who do not find relief with over-the-counter options.
- Cortisone shots, which can provide temporary relief by reducing inflammation in the shoulder joint.
Each of these options offers varying degrees of relief and potential side effects. It’s important to discuss with your orthopedic surgeon to determine the best course of treatment for your specific situation. Because shoulders are more complex than most total joints, I recommend that you visit an orthopedic surgeon who specializes in shoulders to help achieve the best outcomes.
Additionally, supplements such as vitamin D, glucosamine, and chondroitin may be explored, with a healthcare provider’s guidance on their benefits and interactions with other medications.
Surgical Treatment Options for Shoulder Arthritis
Surgical interventions, such as shoulder surgery, for shoulder arthritis are considered when non-surgical treatments fail to provide adequate relief. The decision to proceed with surgery is a significant one, influenced by factors like age and the severity of the condition.
These options, namely arthroscopic debridement, and shoulder joint replacement, promise a more definitive reprieve from the discomforts of shoulder arthritis.
Arthroscopic Debridement
Arthroscopic debridement is a minimally invasive surgical procedure aimed at providing temporary relief from shoulder arthritis pain. It involves the removal of bone spurs and damaged tissue using an arthroscope, a slender instrument fitted with a camera that offers real-time imagery of the joint’s interior. This procedure, while not a cure, can potentially grant pain relief lasting from 12 to 24 months.
The use of small surgical instruments, guided by the arthroscope’s images, allows for precise debridement with minimal impact on surrounding tissues, resulting in a quicker recovery compared to more invasive surgeries.
Shoulder Joint Replacement
Shoulder joint replacement surgery, also known as shoulder replacement surgery, represents a more long-term solution for those grappling with severe shoulder arthritis. This procedure entails swapping out the damaged parts of the glenohumeral joint with prosthetic components designed to mimic the mechanics of a healthy shoulder. The surgery can take several forms, including a total shoulder replacement or a reverse shoulder replacement, depending on the patient’s specific needs.
Post-surgery, patients undergo a recovery process that includes pain management, wearing a sling, and engaging in physical therapy to regain function and strength in the shoulder. With proper care and maintenance, a prosthetic shoulder joint can offer substantial relief from arthritis symptoms and restore a significant range of motion.
Tips for Living with Shoulder Arthritis
Living with shoulder arthritis demands an adaptive approach to daily life. Practical strategies can help manage the pain and maintain mobility, ensuring that the condition’s impact on day-to-day activities is minimized.
Employing simple yet effective techniques like using ice packs, adjusting sleep positions, and setting up an ergonomic workspace can dramatically improve comfort levels and relieve pain.
Sleep Positioning
Adequate sleep is essential, but shoulder arthritis can make finding a comfortable resting position a nightly struggle. Adjusting sleep positions can significantly reduce pain and prevent additional discomfort during the night.
For side sleepers, lying on the non-affected side with a pillow for arm support can ease pressure on the painful shoulder. Back sleepers might find relief with a wedge elevating the upper body and additional support under the knees. Choosing smooth bedding materials and ensuring a supportive mattress can further aid in achieving a restorative night’s sleep while managing shoulder arthritis.
Ergonomic Workstation Setup
An ergonomic workstation is a powerful ally in the fight against shoulder arthritis pain during work hours. Here are some features to look for:
- Chairs with adjustable armrests and memory foam headrests can promote proper posture, reducing strain on the shoulder.
- Sit-stand desks allow for personalized sitting positions, further minimizing shoulder strain throughout the workday.
- Ensuring that monitors are at eye level and that keyboards and mice are within easy reach can prevent the need to reach or hunch, which can exacerbate shoulder pain.
Incorporating ergonomic accessories, such as specialized mice and keyboards, can also help in reducing the risk of over-rotation of the wrist and associated shoulder strain.
Summary
Throughout this post about shoulder arthritis, we’ve delved into its symptoms, potential diagnoses, and treatment options. Understanding the condition is the first step toward reclaiming the quality of life that arthritis threatens to erode. Whether through lifestyle adjustments, physical therapy, medication, or surgery, there are avenues to alleviate pain and restore mobility.
Frequently Asked Questions
What is the average age for arthritis in the shoulder?
The average age for arthritis in the shoulder is over 50, with 30% of people over 60 being affected by shoulder osteoarthritis.
How do you tell if I have arthritis in my shoulder?
You can tell if you have arthritis in your shoulder if you experience pain, stiffness, and hear grinding, clicking, or cracking in the joint. These are the major signs of shoulder arthritis.
What is involved in a shoulder joint replacement surgery?
Shoulder joint replacement surgery involves replacing damaged parts with prosthetic components, followed by a recovery period that includes pain management, wearing a sling, and physical therapy to regain strength and function. It’s important to follow post-operative instructions carefully to ensure successful recovery.