A glenoid fracture is a break in the part of the shoulder blade that forms the socket for the arm bone. It often happens due to trauma like car accidents or falls. This type of fracture can severely impact shoulder stability and movement.
This post covers the types of glenoid fractures, their causes, how they are diagnosed, and the various treatment options available.
Key Takeaways
- Glenoid fractures account for 10% of scapular fractures and can lead to significant shoulder instability; understanding the injury aids in treatment decisions.
- Non-surgical methods, including immobilization and physical therapy, are effective for about 90% of glenoid fractures, while complex cases may require surgical intervention.
- Consulting a fellowship-trained shoulder surgeon is vital for optimizing treatment outcomes for glenoid fractures, leveraging their specialized expertise in managing complex injuries.
Understanding Glenoid Fractures
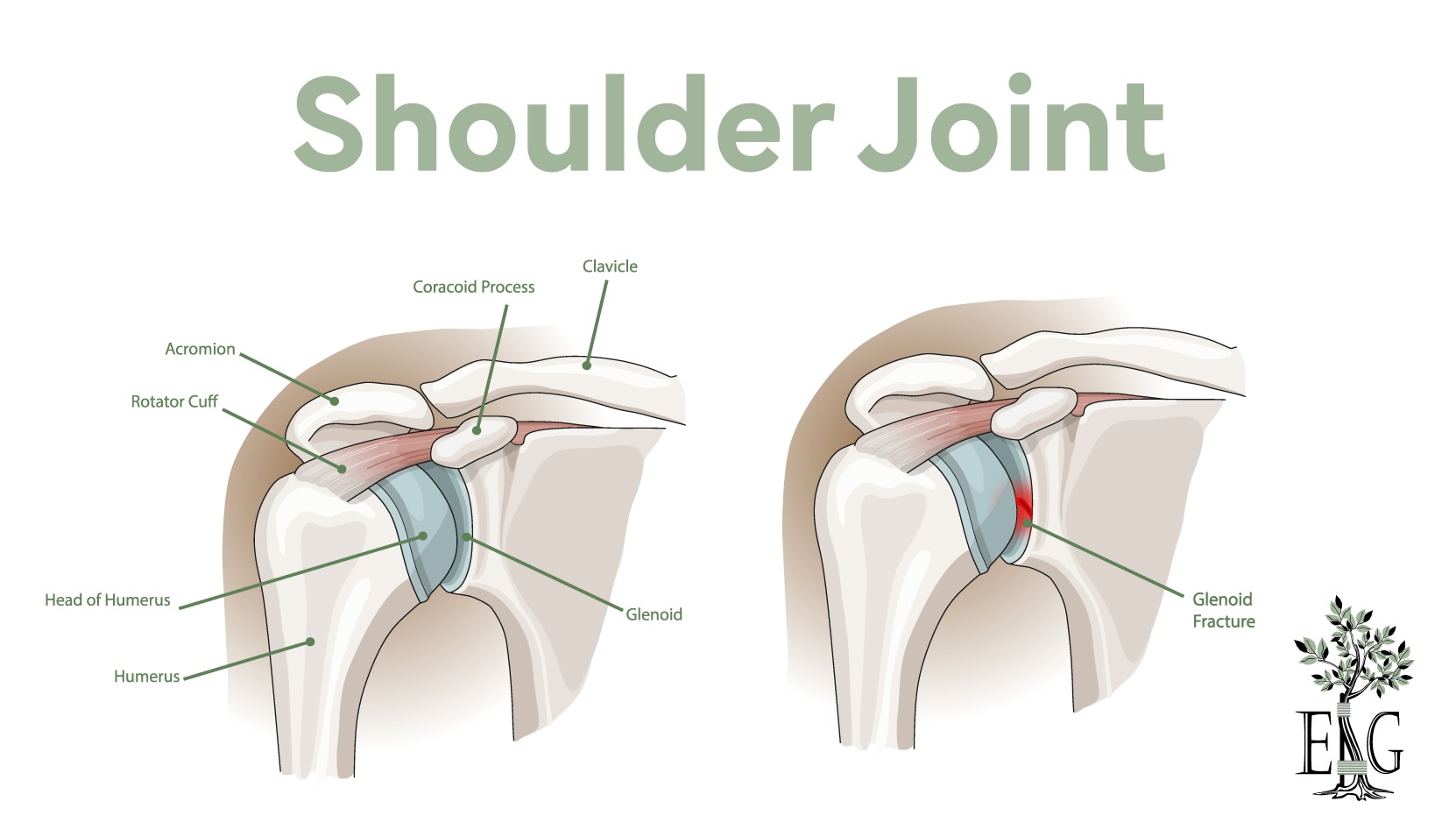
The glenoid is a crucial component of the shoulder joint, acting as the socket that holds the head of the humerus in place. Glenoid fractures, which account for about 10% of all scapular fractures, can significantly affect shoulder stability and movement. When the glenoid is fractured, it disrupts the smooth articulation between the humeral head and the socket, leading to pain and limited mobility.
Recognizing the nature of glenoid fractures benefits both patients and healthcare providers. These fractures can compromise shoulder stability and, if not managed appropriately, may lead to chronic issues. However, with proper treatment, the prognosis is generally good.
Types of Glenoid Fractures
Glenoid fractures are classified based on the mechanism of injury, location, and glenoid fossa fracture pattern.
One common classification is Euler’s, which includes:
- body fractures
- process fractures
- neck fractures
- articular fractures
- combinations of these types
Ideberg’s classification further categorizes glenoid fossa fractures into six types, including avulsions and rim fractures.
Anteroinferior anterior glenoid rim fractures are among the most common types, often associated with traumatic anterior glenohumeral instability events. These rim fractures make up a significant portion of all glenoid fractures, ranging from 75% to 85%. Notably, such anterior glenoid rim fracture is prevalent in older adults following an anterior shoulder dislocation, with a prevalence of 23.2% in patients aged 50 and above.
Non-displaced glenoid fractures, which do not require the bone fragments to be realigned, often heal well with conservative treatment. Conservative management, including immobilization and physical therapy, can be effective for these less severe fractures. For more complex fractures, surgical intervention may be necessary to ensure proper healing and restore shoulder function.
Causes and Risk Factors
High-energy trauma, such as car accidents or significant falls, is the primary cause of glenoid fractures. These types of injuries are often seen in individuals who participate in high-velocity sports or activities that involve a high risk of impact.
Older adults are at a higher risk of glenoid fractures due to weakened and osteoporotic bone, which makes them more susceptible to fractures even from lower-impact incidents like falls. In younger individuals, participation in competitive sports or activities that involve frequent and high-level physical contact increases the risk of such injuries.
Awareness of these risk factors aids in both prevention and effective management of glenoid fractures.
Diagnosis and Imaging Techniques
Accurate diagnosis forms the foundation for effective treatment of glenoid fractures. Identifying these fractures promptly and accurately is essential due to their potential to severely impact shoulder stability and function. The diagnostic process typically begins with a thorough clinical evaluation, including the patient’s history of shoulder instability or previous dislocations.
Imaging studies are pivotal in diagnosing glenoid fractures. X-rays, CT scans, and MRIs are used to visualize the fracture, each offering specific strengths in assessing the injury. These methods help determine the exact location, type, and severity of the fracture, guiding treatment plans effectively.
Physical Examination
A comprehensive physical examination is crucial in initially assessing a potential proximal humerus fracture. This exam includes evaluating the humerus, clavicle, scapula, and shoulder joint, along with checking the active and passive range of motion, strength, and neurovascular status.
Signs indicative of a scapula fractures injury, such as ecchymosis, tenderness to palpation, and impaired range of motion, are carefully noted. The position of the humeral head is also significant; a well-centered humeral head suggests non-operative treatment, whereas subluxation indicates poor future stability.
Imaging Studies
Imaging studies are indispensable in confirming the diagnosis of glenoid fractures. X-rays are typically the first step, with the anteroposterior and axillary views being the most useful for assessing the glenoid fossa. X-rays can reveal fractured bones if the shoulder socket is damaged.
For more detailed visualization, CT scans are often employed. CT scans are superior in assessing the complexity of glenoid fractures, providing a clearer picture of the fracture’s extent and aiding in planning the surgical approach if needed.
Non-Surgical Treatment Options
Non-surgical treatment is often the first line of management for glenoid fractures, especially those that are minimally displaced or nondisplaced. Factors such as the patient’s age, level of function, and social history play a role in determining the appropriate treatment approach.
A significant majority of glenoid fractures, about 90%, do not require surgical intervention and can be treated conservatively. Non-surgical treatment options include the use of slings, splints, or casts to immobilize the shoulder and support the healing process.
Immobilization Methods
Immobilization is a cornerstone of non-surgical treatment for glenoid fractures. Slings, splints, or casts are used to stabilize the shoulder and ensure proper healing of the fracture. This method is particularly effective for avulsion fractures less than 5 mm, where stabilization can prevent further displacement and aid in recovery.
Physical Therapy
Physical therapy helps in regaining mobility and strength after immobilization. Following non-surgical treatment, physical therapy helps restore the shoulder’s range of motion and prevent stiffness. Initial therapy often involves gentle movements to maintain some level of activity in the shoulder, followed by more intensive exercises as healing progresses.
Maintaining an appropriate range of motion prevents long-term stiffness and ensures full recovery. The therapy regimen typically progresses from passive range-of-motion exercises to active and strengthening exercises, designed to restore full function and strength to the shoulder.
Surgical Treatment Approaches
Surgical intervention is often necessary for unstable or significantly displaced glenoid fractures. The decision to undergo surgical treatment depends on the degree of instability and the presence of associated injuries such as rotator cuff tears.
Different surgical techniques are employed based on the fracture’s complexity and location. Open reduction and internal fixation are typically required for significantly displaced fractures, ensuring proper alignment and stability of the shoulder joint.
Fellowship-trained shoulder surgeons are particularly adept at performing these complex procedures, enhancing treatment outcomes.
Arthroscopic Fixation
Arthroscopic fixation techniques offer a minimally invasive approach to treating certain types of glenoid fractures. These methods involve small incisions and the use of specialized instruments to repair the fracture, resulting in faster recovery times and less postoperative pain.
Arthroscopy also allows for the identification and treatment of additional injuries, such as rotator cuff pathology, which can be addressed simultaneously. However, the success of arthroscopic fixation can depend on the size of the bony fragments and the surgeon’s familiarity with complex techniques.
Open Surgical Techniques
Open surgical techniques are often required for more complex glenoid fractures that cannot be adequately addressed through arthroscopy. These methods provide better access to the fracture site, allowing for more precise alignment and stabilization.
Common materials used in open surgery include small plates and screws to secure the bone fragments in place. These techniques are essential for ensuring proper healing and restoring full function to the shoulder joint.
Postoperative Care and Rehabilitation
Postoperative care and rehabilitation are critical to achieving successful outcomes after surgical treatment of glenoid fractures. Regular follow-ups with the orthopedic surgeon help monitor the healing process and address any complications promptly.
Both conservative and operative management can lead to good outcomes, although complications such as chronic shoulder instability and recurrent instability can affect recovery. A comprehensive rehabilitation plan is necessary to restore shoulder function and prevent long-term issues.
Immediate Postoperative Care
In the immediate postoperative period, pain management and passive range of motion exercises are crucial for minimizing discomfort and promoting early recovery. Close radiographic follow-up over several weeks helps ensure that the fracture is healing correctly and identifies any early signs of complications.
In cases of minimally displaced fractures, passive range of motion exercises are recommended to maintain some level of mobility while protecting the healing bone. Routine follow-up care is essential to monitor progress and adjust the treatment plan as needed.
Long-term Rehabilitation
Long-term rehabilitation focuses on gradually restoring full function to the shoulder through a structured exercise program. Patients are advised to begin gentle shoulder exercises within the first 72 hours after surgery to prevent stiffness.
Rehabilitation typically progresses from passive movements to active range-of-motion exercises and eventually to strengthening exercises as healing advances. Achieving a full return to shoulder function can take up to a year, with physical therapy playing a crucial role in this process.
Complications and Risk Management
Managing potential complications is a vital aspect of treating glenoid fractures. Common complications include infection, shoulder stiffness, and nerve injury, which can arise from both surgical and non-surgical treatments.
Effective risk management involves careful surgical technique, adherence to rehabilitation protocols, and regular follow-up appointments to monitor the patient’s progress and address any issues promptly.
Common Complications
Infection is a serious complication that can occur post-surgery, requiring prompt diagnosis and treatment to prevent further issues. Shoulder stiffness, resulting from both surgical and non-surgical treatments, can lead to decreased range of motion if not addressed appropriately.
Nerve injury is another potential complication during surgical interventions, particularly during percutaneous screw fixation. Persistent pain and other issues can also affect recovery, making careful monitoring and management essential.
Prevention and Management
Preventing complications involves lifestyle choices and strict adherence to rehabilitation protocols. For instance, smoking cessation is crucial, as smoking can significantly delay fracture healing. Patients are advised to avoid substance abuse, which can decrease healing and increase the likelihood of complications.
Adhering to prescribed rehabilitation protocols and attending all follow-up appointments are essential for preventing complications and ensuring a smooth recovery. Physical therapy, medications for pain and inflammation, and sometimes additional surgical interventions may be necessary to manage complications effectively.
Consulting a Fellowship-Trained Shoulder Surgeon
Consulting a fellowship-trained shoulder surgeon can help ensure optimal treatment outcomes for glenoid fractures. These surgeons possess advanced training and expertise in treating complex shoulder injuries, providing patients with access to the latest surgical techniques and personalized care.
When choosing a shoulder specialist, it’s a good idea to verify their board certification, fellowship training, and experience in glenoid fracture surgeries.
Benefits of Specialized Care
Fellowship-trained shoulder surgeons offer several benefits that have been shown to help patient outcomes. These surgeons have dedicated years to mastering complex procedures, offering specialized expertise and superior care. Patients can benefit from personalized treatment plans tailored to their unique needs and conditions, ensuring the most effective and efficient recovery.
Choosing a fellowship-trained shoulder surgeon means access to advanced surgical techniques, accurate diagnoses, and comprehensive rehabilitation support, all of which contribute to better long-term outcomes. This specialized care can be very beneficial for managing complex shoulder conditions like glenoid fractures.
Summary
In summary, glenoid fractures are complex injuries that significantly impact shoulder stability and function. Proper diagnosis and treatment are essential for achieving optimal outcomes and preventing long-term complications. Both non-surgical and surgical treatment options are available, depending on the severity and type of fracture.
Consulting a fellowship-trained shoulder surgeon ensures access to advanced techniques and personalized care, enhancing recovery and long-term outcomes. By understanding the nature of glenoid fractures and the various treatment options, patients can make informed decisions and take active steps toward a successful recovery.
Frequently Asked Questions
What are the common causes of glenoid fractures?
Glenoid fractures are commonly caused by high-energy trauma, including car accidents and falls, as well as high-velocity sports injuries. Understanding these causes can aid in prevention and prompt treatment.
How are glenoid fractures diagnosed?
Glenoid fractures are diagnosed through a comprehensive clinical evaluation combined with imaging studies such as X-rays and CT scans, which help assess the fracture’s location, type, and severity effectively.
What are the non-surgical treatment options for glenoid fractures?
Non-surgical treatment options for glenoid fractures primarily involve immobilization with slings or splints, followed by physical therapy to enhance mobility and strength. These approaches facilitate healing while minimizing the need for surgical intervention.
Why is it important to consult a fellowship-trained shoulder surgeon for glenoid fractures?
Consulting a fellowship-trained shoulder surgeon for glenoid fractures is crucial due to their specialized expertise and advanced techniques tailored to complex shoulder injuries, which significantly enhance the potential for optimal recovery and outcomes. Their focused training ensures you receive the best care possible.
What are the potential complications of glenoid fracture treatments?
Potential complications of glenoid fracture treatments include infection, shoulder stiffness, and nerve injury, regardless of whether the approach is surgical or non-surgical. It is crucial to monitor for these issues during recovery.