Menopause often brings unexpected changes, one of which is menopause frozen shoulder. This painful condition, marked by stiff and limited shoulder movement, is more common during menopause due to hormonal changes. Understanding this link is can help for better managing the condition effectively.
In this post, we explore the connection between menopause and menopause frozen shoulder, discuss symptoms, risk factors, and treatment options.
Key Takeaways
- Frozen shoulder, or adhesive capsulitis, is more common in menopausal women due to hormonal changes that increase shoulder pain and stiffness.
- Early diagnosis through physical assessment and imaging is important for effective treatment of frozen shoulder, which can include physical therapy and medication.
- Hormone replacement therapy (HRT) may actually reduce the risk of frozen shoulder in menopausal women by alleviating estrogen deficiency-related joint issues.
Understanding Frozen Shoulder and Its Connection to Menopause
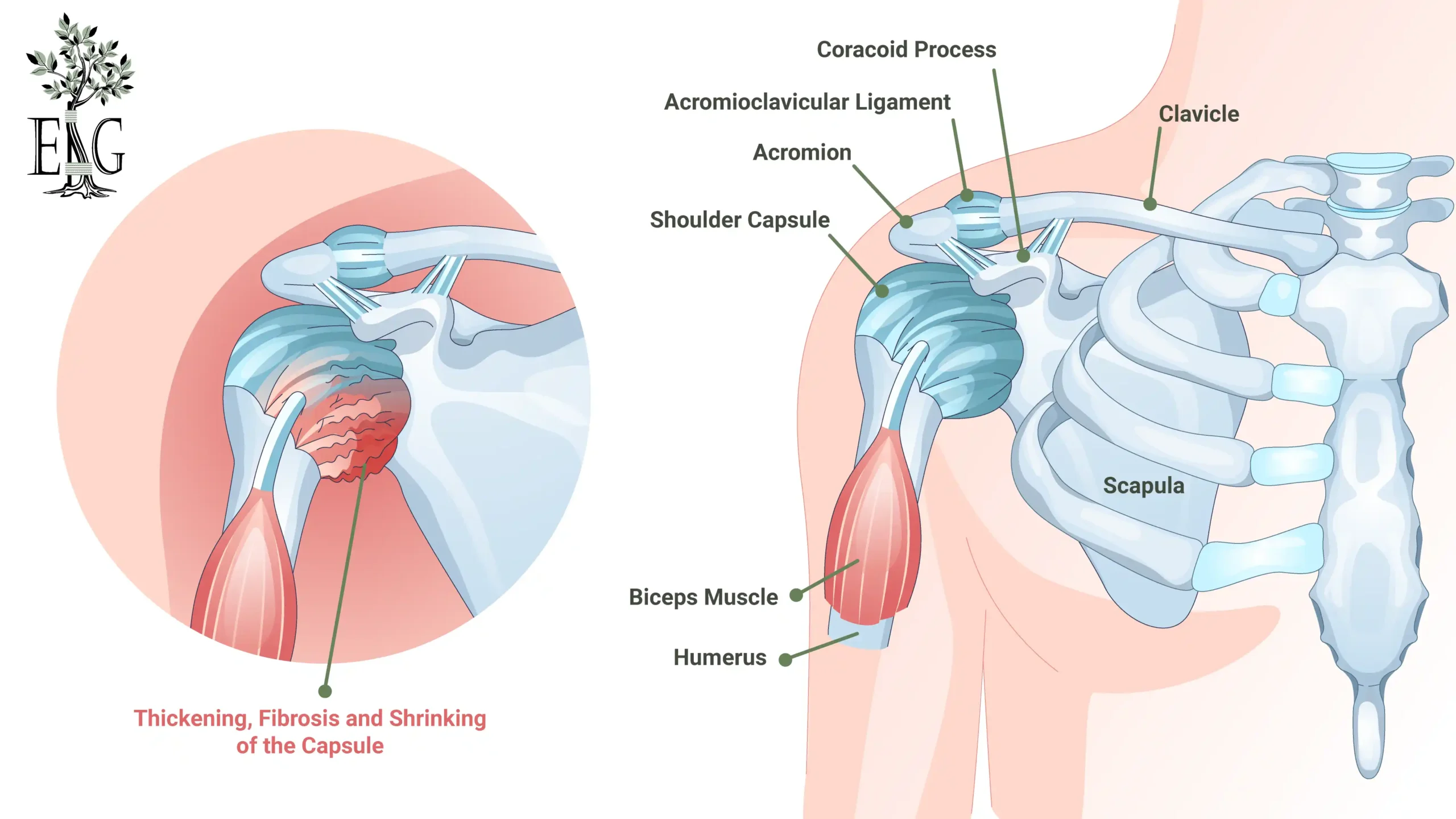
Frozen shoulder, also known as adhesive capsulitis, is a condition characterized by pain and stiffness in the shoulder joint, resulting in limited movement. For menopausal women, the onset of frozen shoulders can be particularly troubling. Hormonal changes during menopause, such as fluctuations and reductions in oestradiol, progesterone, and testosterone, are significant contributors to the development of frozen shoulder. These hormonal shifts are not just minor inconveniences but can profoundly affect joint health and mobility.
Interestingly, while there is no conclusive evidence of a direct link between menopause and frozen shoulder, the incidence of frozen shoulder is notably higher among women in menopause compared to other life stages. This heightened risk is attributed to the hormonal changes that occur during menopause, which can exacerbate shoulder symptoms, including pain and stiffness in the muscles and joints.
Thus, understanding the interplay between menopause and frozen shoulder is crucial for effective management and relief.
Symptoms of Frozen Shoulder
The symptoms of frozen shoulder can be both debilitating and frustrating, often making simple daily tasks seem insurmountable. Common symptoms include pain, stiffness, and a significant restriction in shoulder movement. For menopausal women, these symptoms can be especially intense, adding to daily challenges and creating a sense of heaviness in the arm. Nighttime discomfort often disrupts sleep, adding to the challenges faced during the day.
Dressing, reaching overhead, and even combing hair can become challenging as the shoulder capsule thickens and restricts shoulder motion. Patients often feel as though their arm is stuck, with both active and passive movements of the shoulder joint limited. This shoulder pain and stiffness significantly hinder shoulder mobility, so recognizing these symptoms early is crucial for better treatment outcomes.
Risk Factors for Frozen Shoulder During Menopause
Menopausal women are at a higher risk of developing frozen shoulder compared to other groups, primarily due to the drop in estrogen levels that occurs during menopause. Hormonal changes during this period can significantly increase the risk of developing frozen shoulder, making it a common concern among women aged 40 to 60. The interplay of these hormonal changes with other risk factors creates a perfect storm for the onset of frozen shoulder.
Certain medical conditions, such as cervical spondylosis, can also elevate the risk of developing frozen shoulder. Additionally, individuals who have previously injured their shoulders or have undergone shoulder surgery are at a higher risk of experiencing this condition. High triglyceride levels and stress related to life changes, commonly experienced during menopause, further contribute to the risk of frozen shoulder. Understanding these risk factors can help in taking preventive measures and seeking timely treatment.
For many women, the 40 to 60 age range is already a period of significant stress and life changes, which can exacerbate the risk factors for frozen shoulder. Recognizing these risks and understanding their interplay with menopausal symptoms is crucial for early diagnosis and effective management of frozen shoulder.
Diagnosing Frozen Shoulder
Diagnosing frozen shoulder typically involves a thorough assessment of the patient’s medical history, symptoms, and a physical examination to evaluate range of motion. This physical examination may be challenging due to the stiffness associated with frozen shoulder, making it difficult to move the arm. Accurate diagnose frozen shoulder is important for effective treatment and management, ensuring that the condition is correctly identified and not mistaken for other shoulder issues. It is recommended to consult a fellowship-trained orthopedic shoulder surgeon, as they have specialized experience and expertise in accurately diagnosing and effectively treating frozen shoulder.
In some cases, magnetic resonance imaging (MRI) may be used to confirm the diagnosis and differentiate frozen shoulder from similar conditions. This imaging test helps to provide a clearer picture of the shoulder joint capsule and the extent of the condition.
Early and precise diagnosis can significantly improve treatment outcomes, allowing for a more targeted and effective approach to managing frozen shoulder.
Treatment Options for Frozen Shoulder
Treating frozen shoulder requires a multifaceted approach to address pain, stiffness, and restricted movement. Common conservative treatments include pain management strategies, physical therapy, and PRP shoulder treatments. These methods aim to alleviate symptoms and gradually improve shoulder mobility. The exact cause of frozen shoulder remains unclear, posing a challenge in determining the most effective treatment.
In addition to these conservative measures, advanced treatments may be necessary for more severe cases. These can include surgical interventions and injection treatments, which can provide significant relief and improve shoulder function.
Physical Therapy
Physical therapy is a cornerstone in treating frozen shoulder, aiming to restore, maintain, and promote physical function. During the freezing stage, exercises focus on pain management and reducing inflammation. In the frozen and thawing stages, the emphasis shifts to restoring joint mobility and improving range of motion. Stretching exercises are particularly crucial, helping to combat the stiffness and improve joint mobility.
Consult a doctor or physical therapist before starting any new stretching routine to ensure safety and effectiveness. Combining physical therapy with anti-inflammatory medications can enhance outcomes, providing better pain relief and promoting joint health.
Medication and Pain Management
Medication and pain management are key components in treating frozen shoulder. Commonly recommended medications include NSAIDs, oral corticosteroids, and corticosteroid injections, which can effectively reduce pain and inflammation. These medications play a crucial role in managing the discomfort associated with frozen shoulder, helping patients to engage more fully in physical therapy and other treatment options.
Pain management strategies play an important role for relief and aiding in overall recovery and management of frozen shoulder symptoms. Early pain management can significantly improve quality of life and facilitate better treatment outcomes.
Platelet Rich Plasma (PRP)
Platelet-Rich Plasma (PRP) has shown promising results in treating frozen shoulder. For the right patients, PRP injections can help reduce inflammation and pain in the shoulder joint, promoting faster recovery. Many patients report a significant decrease in pain levels following PRP treatments for frozen shoulder, as well as improved mobility.
Advanced Treatments
In severe cases of frozen shoulder, advanced treatments may be necessary. Surgical options include shoulder manipulation and arthroscopy, which can provide significant relief and improve shoulder function. Keyhole surgery, often performed under light general anaesthesia, is a common procedure for frozen shoulder, allowing patients to regain movement and reduce pain.
After surgery, patients are encouraged to use their arm to maintain the movement achieved during the procedure. These advanced treatments are crucial for those who do not respond to conservative measures, offering a pathway to recovery and improved quality of life.
Hormone Replacement Therapy (HRT) and Frozen Shoulder
Hormone replacement therapy (HRT) can play a significant role in managing frozen shoulder during menopause. The decrease in estrogen levels during menopause can lead to reduced production of synovial fluid, which lubricates joints, contributing to the development of frozen shoulder. Estrogen replacement through HRT may help mitigate these issues, potentially decreasing the risk of frozen shoulder.
Research indicates that women not receiving HRT are significantly more likely to develop frozen shoulder compared to those who do. Despite these promising findings, further studies with larger participant groups are essential to confirm the protective effects of HRT against frozen shoulder.
For menopausal women, hormone replacing therapy may provide a valuable option in reducing the risk and managing the symptoms of frozen shoulder.
Lifestyle Modifications and Prevention
Lifestyle modifications can play a crucial role in preventing frozen shoulder. Lack of physical activity can worsen muscle weakness and joint stiffness, increasing the risk of developing frozen shoulder. Regular stretching and strengthening exercises for the shoulder can help prevent stiffness and maintain joint mobility.
Maintaining a healthy weight through diet and exercise is also crucial for preventing frozen shoulder in post-menopausal women. Staying active and maintaining flexible shoulder joints can significantly reduce the risk of developing frozen shoulder.
Tips for Sleeping with Frozen Shoulder
Sleeping with a frozen shoulder can be particularly challenging due to the pain and stiffness. One effective strategy is to sleep on your back with pillows under your knees and the affected arm to improve comfort. Avoiding sleeping on the affected shoulder is crucial to prevent increased pain and facilitate healing.
A body pillow can provide full-body support and comfort during sleep. Applying a warm compress before bedtime can help relax shoulder muscles and ease tension. Gentle stretches before bed may also alleviate stiffness and promote better sleep.
Summary
In summary, frozen shoulder during menopause is a challenging condition influenced by hormonal changes and various risk factors. Recognizing the symptoms early and obtaining an accurate diagnosis is crucial for effective treatment. Various treatment options, including physical therapy, medication, and advanced treatments, offer pathways to relief and recovery.
Understanding the potential benefits of hormone replacement therapy and making lifestyle modifications can further help in managing and preventing frozen shoulder. By staying proactive and informed, menopausal women can significantly improve their quality of life and shoulder health.
Frequently Asked Questions
What are the common symptoms of frozen shoulder?
The common symptoms of frozen shoulder are pain, stiffness, and limited shoulder movement, which can significantly hinder daily activities.
How is frozen shoulder diagnosed?
Frozen shoulder is diagnosed through a combination of medical history, symptom assessment, and a physical examination, with MRI potentially used for confirmation.
What treatment options are available for frozen shoulder?
Treatment options for frozen shoulder primarily include physical therapy, medications for pain management, PRP, and in some cases, advanced treatments such as surgery. It’s important to consult with a healthcare professional to determine the most appropriate approach for your situation.
Can hormone replacement therapy help with frozen shoulder?
Hormone replacement therapy may help reduce the risk of developing frozen shoulder by addressing joint health issues related to lower estrogen levels. Therefore, it can be beneficial for individuals experiencing symptoms associated with this condition.
What lifestyle modifications can help prevent frozen shoulder?
To prevent frozen shoulder, engaging in regular physical activity, incorporating stretching and strengthening exercises, and maintaining a healthy weight are all benficial. These lifestyle modifications can significantly reduce your risk.