Reverse shoulder replacement shifts the workload from the rotator cuff muscles to the deltoid muscle. This post covers what happens to rotator cuff muscles after reverse shoulder replacement, including changes in function and recovery essentials.
Key Takeaways
- Reverse shoulder replacement surgery repositions the ball and socket of the shoulder joint, allowing the deltoid muscle to compensate for damaged rotator cuff muscles, thereby improving shoulder function.
- Post-surgery, the deltoid muscle increases in activity and hypertrophies to handle the new functional load, while tailored physical therapy helps mitigate rotator cuff muscle atrophy and improves shoulder mobility.
- While reverse shoulder replacement significantly reduces pain and improves shoulder stability for patients with irreparable rotator cuff tears, it may restrict certain ranges of motion and carries risks such as nerve damage, implant loosening, and complications requiring revision surgery.
Understanding Reverse Shoulder Replacement Surgery
The unique approach or reverse shoulder replacement proves particularly advantageous for those suffering from severe rotator cuff injuries, as traditional shoulder replacements may not yield satisfactory results.
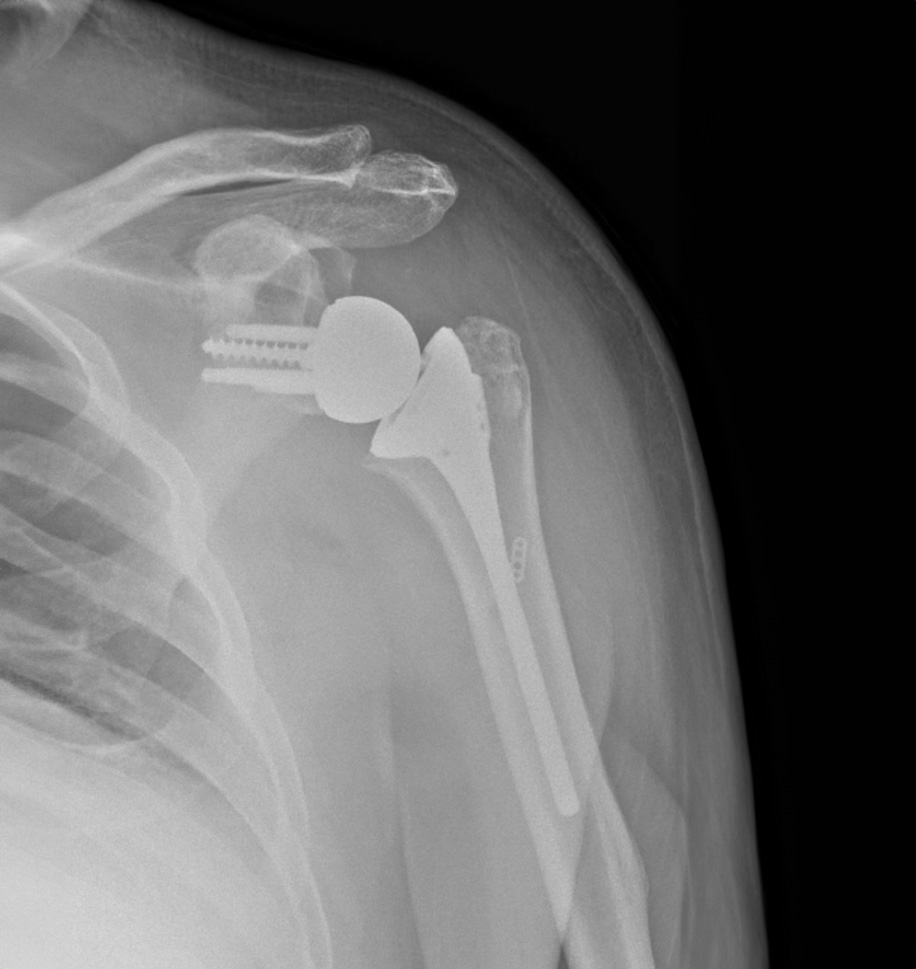
In this procedure, the ball is placed on the socket side of the shoulder joint, and the socket is placed on the arm side, supported by a metal stem in the humerus. This reversal allows the deltoid muscle to lift the arm in cases where the rotator cuff is torn or malfunctioning. It’s a special type of shoulder surgery designed to replace damaged parts with artificial components, ensuring better shoulder function for those with specific injuries.
Reverse shoulder surgery can prove to be a gamechanger for patients with severe pain and shoulder weakness unresponsive to other treatments. It is often recommended for conditions like rotator cuff tear arthropathy, where the rotator cuff tendons are severely damaged or absent. By improving the physics in the shoulder, this surgery doubles the lever arm of the deltoid muscle, maintaining the fulcrum in the optimum position to allow arm movement.
Indications for Reverse Shoulder Replacement
Reverse total shoulder replacement is recommended for various conditions where shoulder function is severely compromised and nonsurgical treatments have not been effective. One common indication is irreparable rotator cuff damage that leads to painful arthritis or significant functional problems. In such cases, the traditional shoulder replacement may not provide sufficient relief or functionality.
Complex fractures of the proximal humerus, particularly those near the ball of the humerus that are broken into multiple pieces, can necessitate the use of a reverse prosthesis. This surgery is particularly beneficial for patients with large rotator cuff tears and rotator cuff tear arthropathy, as it allows different muscles, especially the deltoid, to take over shoulder function and provide stability.
Role of Rotator Cuff Muscles in Shoulder Function
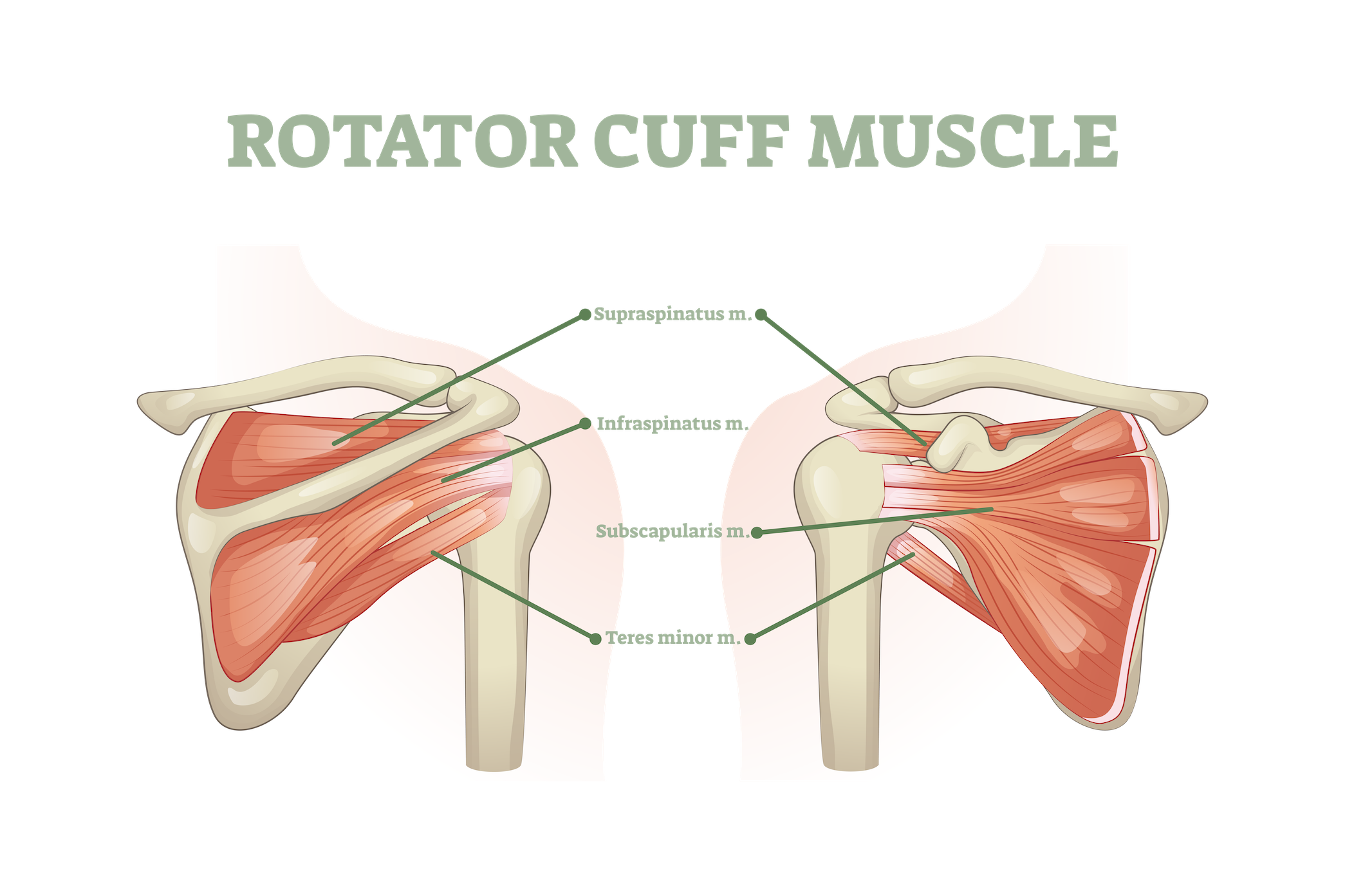
The rotator cuff muscles serve a pivotal role in providing stability to the shoulder joint during movement. These muscles include:
- Supraspinatus
- Infraspinatus
- Teres minor
- Subscapularis
They are essential for not only maintaining the stability of the shoulder joint but also enabling a wide range of arm motions.
Given their role in facilitating actions like lifting and rotating the arm, the rotator cuff muscles are integral to everyday activities. Understanding their anatomy and function is vital to grasp the impact of rotator cuff tears and the subsequent changes that occur post-surgery.
The supraspinatus muscle, connected to the upper arm bone, initiates the abduction of the arm, thereby enabling you to lift your arm away from your body.
The infraspinatus and teres minor muscles support the shoulder’s external rotation, allowing for outward rotation of the arm. Concurrently, the subscapularis muscle facilitates the shoulder’s internal rotation, enabling inward rotation of the arm. Together, these muscles work harmoniously to ensure smooth and stable shoulder movements.
Impact of Rotator Cuff Tears
Tears in the rotator cuff muscles, includinga large rotator cuff tear, can lead to significant shoulder pain and reduced arm strength. These injuries impair the ability to lift the arm or perform overhead activities, severely limiting daily functions. Patients with chronic rotator cuff tears often experience increased activity of the posterior deltoid and biceps brachii muscles during upward movements, as these muscles try to compensate for the torn rotator cuff.
Additionally, patients with rotator cuff tears show decreased activity of the posterior deltoid during the downward phase of movements compared to controls, further highlighting the functional impairment caused by these injuries.
Changes to Rotator Cuff Muscles Post-Surgery
After reverse shoulder replacement surgery, the function of rotator cuff muscles typically diminishes, necessitating compensatory mechanisms from other muscles. The deltoid muscle, in particular, takes over much of the load previously managed by the rotator cuff, adapting to its new role in shoulder function.
This shift in muscle dynamics is crucial for understanding the overall recovery process and the importance of targeted rehabilitation strategies to ensure optimal outcomes post-surgery.
Muscle Adaptation and Compensation
Post-surgery, the deltoid muscle adapts by increasing its activity to compensate for the loss of functional rotator cuff muscles. This adaptation often involves hypertrophy, where the deltoid muscle enlarges to better handle the increased workload.
The deltoid muscle’s role becomes critical in shoulder elevation and overall function, taking over the primary function of lifting the arm. Specific training of the posterior deltoid might help compensate for deficient rotator cuff muscles, particularly in patients with chronic rotator cuff tears.
Muscle Atrophy and Recovery
Causes of muscle atrophy in the rotator cuff after surgery include:
- Reduced activation
- Altered load distribution
- Reduced use
- Altered biomechanics of the shoulder joint post-surgery
Recovery strategies for atrophied rotator cuff muscles often include tailored physical therapy to gradually restore strength and prevent further deterioration. Structured physical therapy programs help in reducing muscle atrophy and improving overall shoulder mobility and strength post-surgery.
Role of Physical Therapy
Following reverse shoulder replacement, physical therapy becomes vital to optimize muscle function with a focus on the deltoid and the remaining rotator cuff muscles. Formal physical therapy programs are recommended to strengthen the shoulder and improve flexibility following surgery.
These sessions aim at strengthening the shoulder and enhancing range of motion – key elements for a successful recovery. By adhering to a structured physical therapy regimen, patients can significantly enhance their post-surgery outcomes and regain functional use of their shoulders.
Benefits and Limitations of Reverse Shoulder Replacement
With a high success rate, reverse shoulder replacements allow most patients to return to their normal lifestyle with full functionality within a few months. This surgery is particularly effective for patients with irreparable rotator cuff tears, providing them with much-needed shoulder stability.
Nevertheless, understanding both the advantages and limitations of this procedure is key for setting realistic expectations and preparing for the impending recovery journey.
Pain Relief and Improved Function
Reverse shoulder replacement surgery aims to significantly reduce pain and improve shoulder function for patients suffering from severe shoulder issues. This procedure often results in dramatic improvement from preoperative to postoperative function, significantly reducing pain during everyday activities.
Patients typically experience considerable pain relief following the surgery, allowing them to return to a normal, pain-free life and restore their ability to lead an active lifestyle.
Limitations in Range of Motion
The primary limitation of reverse shoulder replacement lies in the potential restriction of range of motion after the surgery. The mechanical constraints of the procedure can slightly restrict the range of motion compared to a natural shoulder.
Patients may experience reduced strength in internal rotation and overhead lifting, with persistent limitations in certain directions of shoulder movement, such as behind the back. Therapeutic exercises are essential to improve range of motion and functional use of the shoulder, which are critical for successful recovery.
Risks and Complications
As with all joint replacement surgeries, reverse shoulder replacement comes with certain risks and possible complications. These include issues such as:
- Bleeding
- Nerve damage
- Infection
- Wear
- Loosening of the implant
- Dislocation of components
It is crucial to understand that these risks may be higher in individuals undergoing repeat surgeries due to the complexity involved. If you are able to, please have your surgery performed by a fellowship-trained shoulder surgeon, as they undergo advanced training for shoulder replacement.
Nerve Injury and Muscle Weakness
Nerve injuries during reverse shoulder arthroplasty can be caused by:
- Surgical transection
- Compression from retractors
- Damage from nerve blocks
- Excessive arm traction
- Postoperative hematoma pressure
These injuries can affect muscle strength and coordination, but most cases resolve independently without long-term effects.
Axillary nerve injuries are particularly concerning in reverse shoulder arthroplasty due to the deltoid muscle’s reliance on this nerve. Fortunately, most nerve injuries resolve without long-term effects, allowing patients to regain muscle strength and coordination over time.
Implant Loosening and Revision Surgery
Implant loosening, a significant issue requiring revision surgeries, can be exacerbated by factors such as infection or poor bone quality. Mechanical instability and wear can also lead to implant loosening, necessitating further surgical interventions.
Revision surgery is more complex and carries a higher risk of complications than the initial replacement. In complex cases, revision surgery might involve bone grafting or changing the implant design. The risk of developing complications increases with revision surgeries, underlining the importance of thorough planning and consultation with a shoulder surgeon.
Preparing for Surgery
Preparation for reverse shoulder replacement surgery entails various important steps, encompassing medical evaluations, imaging tests, and readiness at home. Patients should ask their doctor about medical history, medications, tobacco use, and post-surgery care, including the use of a sling (immobilizer), bathing, eating, and medication instructions.
It’s important for patients to disclose all medications they are currently taking to their doctor, which includes over-the-counter drugs, herbs, and supplements. It’s recommended to wear loose-fitting clothes and a button-front shirt to the hospital, and patients should not eat or drink after midnight the night before the surgery.
Medical Evaluation and Imaging Tests
Imaging tests such as X-rays may be needed before surgery to provide a clear view of the shoulder joint. A CT scan might be performed to provide detailed images of the bones, while an MRI might be used to evaluate the soft tissue around the bones.
Home Preparation and Support
Ensuring all essential items are easily accessible to avoid unnecessary reaching or stretching is critical. Patients should arrange for physical assistance during the initial recovery period after the surgery, including help with daily tasks like dressing and cooking.
Post-Surgery Recovery Process
The recovery journey post reverse shoulder replacement surgery encompasses immediate post-operative care as well as prolonged rehabilitation. Within a few days after surgery, most patients are given the green light to use their arm for daily activities, and they usually commence with physical therapy and recovery-oriented exercises at home.
Keeping all follow-up appointments with the provider can help achieve the best possible outcome after reverse shoulder replacement surgery. Patients should be prepared for a recovery period that can last between 4 to 8 months, depending on individual progress and adherence to rehabilitation protocols.
Immediate Post-Operative Care
Immediately following surgery, the arm will be placed in a sling or brace. Patients rest in a recovery area for a short time and undergo X-rays to ensure proper placement of the implant.
To manage short-term pain after surgery, medications such as opioids, nonsteroidal anti-inflammatory drugs (NSAIDs), and local anesthetics are often prescribed.
Long-Term Rehabilitation
Recovery from reverse shoulder replacement surgery typically takes between 4 to 8 months. Common at-home exercises include gently swinging the arm, walking fingers up a wall, and shoulder rotations.
Formal physical therapy sessions are essential in helping regain shoulder strength and motion after surgery.
Lifespan of the Reverse Prosthesis
Generally, a reverse prosthesis has a long lifespan, with about 90% of shoulder replacements remaining intact a decade post-surgery and roughly 80% still functional two decades after the surgery. Factors such as the design of the implant and whether components are cemented or cementless can influence the longevity of the prosthesis.

Younger patients tend to have a shorter lifespan for shoulder prostheses due to higher demands on the implant. Nonetheless, the reverse shoulder replacement has proven to be a durable solution for many, providing significant benefits such as:
- Pain relief
- Improved function
- Increased range of motion
- Enhanced stability
These benefits can last for years, improving the quality of life for patients.
Summary
Reverse shoulder replacement surgery offers a viable solution for patients with severe shoulder pain and dysfunction, especially those with irreparable rotator cuff tears. By reversing the ball and socket structure, this surgery enables the deltoid muscle to compensate for the loss of rotator cuff function, providing stability and improved shoulder mobility.
Understanding the changes that occur in the rotator cuff muscles post-surgery, including muscle adaptation, atrophy, and the role of physical therapy, can be helpful for a successful recovery. While there are risks and limitations associated with the surgery, the benefits often outweigh these challenges, allowing patients the opportunity to lead a pain-free and active lifestyle.
Frequently Asked Questions
Who is a candidate for reverse shoulder replacement surgery?
Patients with irreparable rotator cuff damage, severe shoulder pain, complex fractures of the proximal humerus, and rotator cuff tear arthropathy are considered candidates for reverse shoulder replacement surgery. This option should be discussed with a healthcare professional to determine the best course of action.
What are the risks associated with reverse shoulder replacement surgery?
The risks associated with reverse shoulder replacement surgery include bleeding, nerve damage, infection, implant loosening, and dislocation of components, with specific concerns for nerve injuries and implant loosening. For the best results, it’s advisable to see a fellowship-trained shoulder surgeon.
How long is the recovery period after reverse shoulder replacement surgery?
The recovery period after reverse shoulder replacement surgery generally takes between 4 to 8 months, with patients beginning physical therapy and gentle exercises at home soon after the procedure.