Hip bursitis is an often painful condition that can significantly impact daily life, making simple movements like walking, standing, or even sleeping a challenge. For those experiencing this discomfort, one of the most pressing questions is, “How long will this last?”
The answer isn’t always straightforward, as the duration of hip bursitis can vary widely depending on its underlying causes, the severity of inflammation, and the effectiveness of treatment. In this post, we’ll offer insights into its causes, symptoms, diagnosis, and various treatment approaches.
Key Takeaways
- Hip bursitis can last from a few weeks to several months, and in some cases, even longer, depending on the cause and treatment adherence.
- Common causes include overuse, repetitive motions, direct injury, underlying conditions like arthritis or leg length discrepancies, and poor posture.
- Many cases respond well to non-surgical methods such as rest, ice, medications, and physical therapy, while surgical intervention may be considered for persistent cases.
What is Hip Bursitis?
To understand hip bursitis, it’s essential to first understand the role of bursae. Bursae are small, fluid-filled sacs located throughout the body, acting as cushions between bones, tendons, and muscles. Their primary function is to reduce friction and allow for smooth movement of joints. When these bursae become inflamed, the condition is known as bursitis.
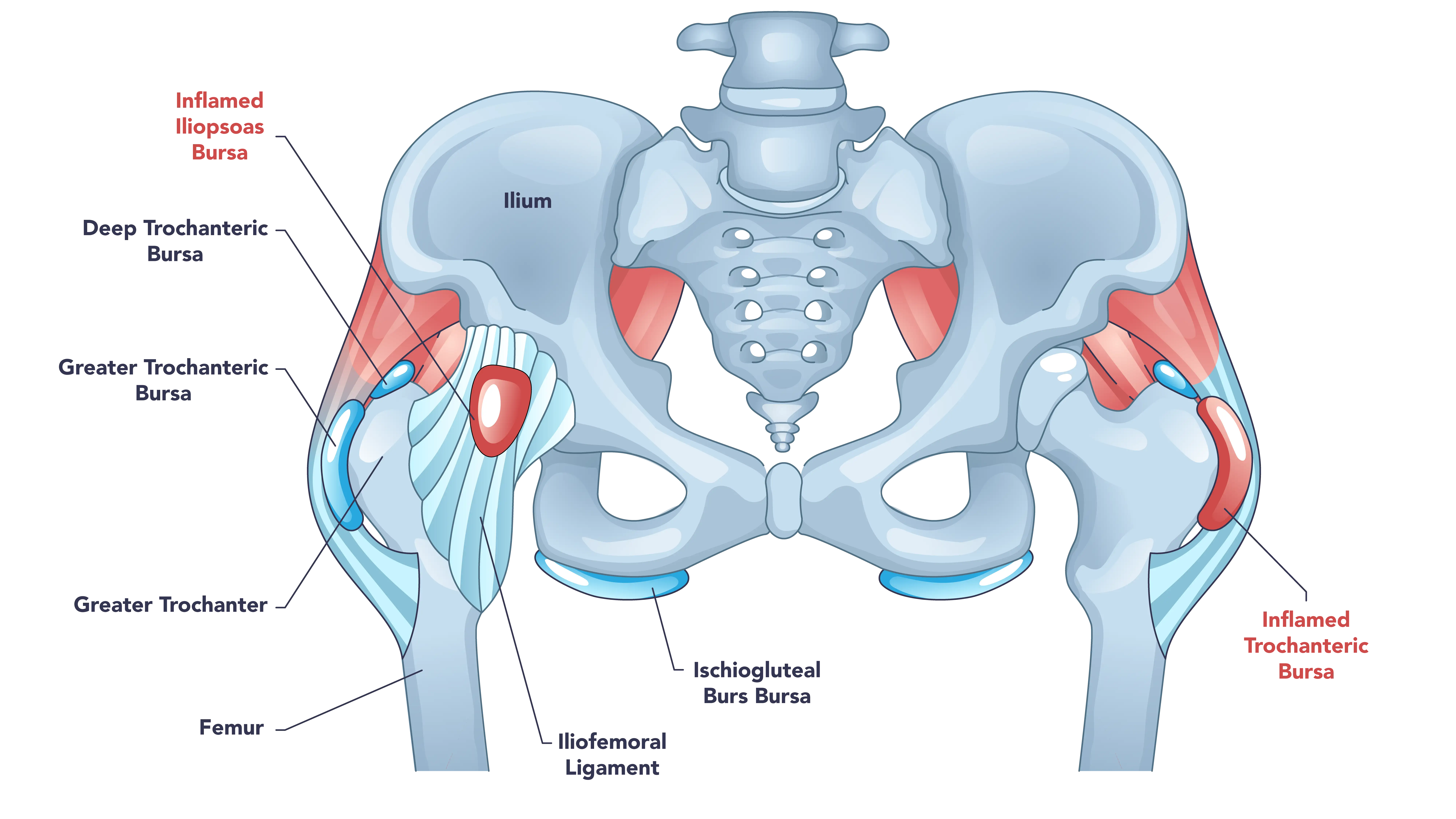
In the hip, there are two main bursae that can become inflamed:
- Trochanteric Bursa: This is the most commonly affected bursa in the hip. It’s located on the outer side of the hip. Inflammation of this bursa leads to trochanteric bursitis, often causing pain on the outside of the hip.
- Iliopsoas Bursa: Situated on the inside of the hip, near the groin, this bursa can also become inflamed, leading to iliopsoas bursitis. This type typically causes pain around the groin area.
When a bursa becomes inflamed, the fluid inside it can increase, causing swelling, pain, and tenderness in the affected area. This inflammation can make even simple movements painful and restrict the hip’s range of motion.
Causes of Hip Bursitis
Hip bursitis can develop due to a combination of factors, ranging from acute injury to chronic overuse and underlying medical conditions. Understanding these causes supports effective treatment and prevention.
1. Repetitive Motion and Overuse
One of the most common culprits behind hip bursitis is repetitive motion or overuse of the hip joint. Activities that involve repeated hip movements can irritate the bursae over time. These may include running, cycling, stair climbing, and standing for prolonged periods of time. Additionally, poor form during exercises or sports can exacerbate stress on the hip.
2. Direct Injury to the Hip
An acute injury can directly inflame a bursa. This might occur from falls, bumping the hip against a hard surface, or lying on one side for an extended period.
3. Underlying Medical Conditions
Several systemic conditions may increase the risk of developing bursitis, including hip arthritis, diabetes, and thyroid disease.
4. Biomechanical Issues and Postural Problems
Structural or biomechanical imbalances can alter the mechanics of the hip joint, leading to increased friction and pressure on the bursae:
- Leg Length Discrepancy: When one leg is noticeably shorter than the other, it can cause an uneven gait and place abnormal stress on the longer hip.
- Scoliosis: Curvature of the spine can affect posture and hip alignment, contributing to bursitis.
- Bone Spurs: Bony growths on the hip bone can rub against the bursa, causing irritation.
- Weak Hip Muscles: Insufficient strength in the hip abductor muscles can lead to improper hip mechanics and increased strain on the bursa.
- Tight IT Band: A tight iliotibial (IT) band, a thick band of tissue running along the outside of the thigh, can increase friction over the trochanteric bursa.
Symptoms of Hip Bursitis
The symptoms of hip bursitis can range from mild to severe and may develop gradually, worsening over time. The most common symptom is pain around the hip area. This pain is often felt on the outer side of the hip (for trochanteric bursitis) or in the groin area (for iliopsoas bursitis).
Initially, the pain may feel sharp and intense. Over time, it may become a dull ache. It typically worsens with activities that involve the hip, such as walking, climbing stairs, lying on the affected side at night, and prolonged standing.
It’s important to note that hip pain can stem from various conditions, so a proper diagnosis is often essential to differentiate bursitis from other issues like tendonitis, arthritis, or muscle strains.
Diagnosis of Hip Bursitis
Diagnosing hip bursitis typically involves a combination of a thorough medical history, physical examination, and sometimes imaging tests to rule out other conditions.
Your doctor will likely start by asking about your symptoms, activity levels, and any previous injuries or medical conditions. The affected hip will then likely be examined and checked for swelling and range of motion. Your doctor may press on the hip to check for tenderness.
Imaging tests may be utilized to confirm the diagnosis. While X-rays cannot visualize bursae, they are often used to rule out other potential problems, such as hip fractures, arthritis, or bone spurs. Magnetic resonance imaging (MRI) can provide detailed images of soft tissues, including the bursae, and can generally confirm inflammation or identify other soft tissue injuries.
Treatment Options for Hip Bursitis
Many cases of hip bursitis respond well to conservative, non-surgical treatments. The primary goals of treatment are to reduce pain and inflammation, restore normal hip function, and prevent recurrence. An experienced hip specialist can evaluate the condition and help guide the most appropriate treatment path.
Conservative Treatments
- Rest and Activity Modification: This is often the first step. Avoiding activities that aggravate the pain, such as prolonged standing, running, or lying on the affected side, can allow the bursa to heal.
- Ice Application: Applying ice packs to the affected area for 15-20 minutes several times a day may help reduce inflammation and pain.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Over-the-counter NSAIDs may be used to reduce pain and inflammation.
- Physical Therapy: A tailored physical therapy program may be highly beneficial. A physical therapist can guide you through stretching, strengthening, and gait correction exercises, personalized to your needs. These exercises can improve flexibility and strength.
- Assistive Devices: Using a cane or crutches temporarily may reduce pressure on the hip while walking.
Surgical Treatment
Surgery for hip bursitis is rare and is typically considered only when conservative treatments have failed to provide relief after an extended period. In some cases, the inflamed bursa may need to be removed. This can often be done arthroscopically, a minimally invasive technique that uses small incisions and a camera.
Recovery Timeline for Hip Bursitis
This is the central question for many patients, and the answer is highly individual. The duration of hip bursitis can range from a few days to several months, and in some cases, even longer. It largely depends on whether the condition is acute or chronic, the underlying cause, the severity of inflammation, and how diligently the patient adheres to the treatment plan.
Acute Bursitis
Acute hip bursitis typically flares up suddenly, likely due to a specific injury or a short period of overuse. Many individuals experience significant improvement within a few days to a couple of weeks with conservative care. The initial sharp pain may subside, transitioning to a dull ache. For many patients, resolution of symptoms and return to normal activities can often be achieved within 4 to 6 weeks if the patient diligently follows their treatment plan and avoids aggravating activities.
Chronic Bursitis
Chronic hip bursitis develops when the inflammation persists over a longer period or recurs frequently. This can happen if the underlying cause is not addressed, if treatment is inconsistent, or if the bursa has become thickened over time. Chronic bursitis tends to be more stubborn and can last several weeks to several months.
Additionally, chronic bursitis can go away and come back, especially if the issues that caused it are not fully resolved. In severe or persistent cases, surgery may be considered.
Factors Influencing Duration:
- Severity of Inflammation: More severe inflammation may take longer to resolve.
- Underlying Cause: Bursitis caused by a simple overuse injury might heal faster than that linked to chronic arthritis or significant biomechanical issues.
- Adherence to Treatment: Consistently following rest recommendations, performing physical therapy exercises, and taking medications as prescribed significantly impacts recovery time.
- Lifestyle Changes: Adopting habits that reduce stress on the hip, such as maintaining a healthy weight and using proper body mechanics, can shorten recovery and help prevent recurrence.
Summary
The duration of hip bursitis symptoms can vary significantly, from a few weeks for acute cases to several months for chronic or recurrent issues. Key to a successful and timely recovery is early diagnosis, consistent adherence to a personalized treatment plan, and proactive lifestyle modifications. While surgical intervention is a rare consideration, it offers a possible solution for the most persistent cases. Understanding the causes, recognizing the symptoms, and actively participating in your recovery journey are important. Patience and persistence are your allies in overcoming hip bursitis and returning to an active lifestyle.
Frequently Asked Questions
Can hip bursitis go away on its own?
In many cases, mild acute hip bursitis can improve with rest and avoidance of aggravating activities. However, for more persistent or severe cases, medical intervention and a structured treatment plan are usually important to ensure full recovery and prevent the condition from becoming chronic.
What activities should I avoid if I have hip bursitis?
It’s generally recommended to avoid activities that worsen your hip pain. This may include prolonged standing, running, cycling, climbing stairs, and lying directly on the affected hip. Your doctor and physical therapist can provide specific guidance based on your condition.
How can I sleep comfortably with hip bursitis?
If you have trochanteric bursitis, it may help to avoid sleeping on the affected side. Placing a pillow between your knees when sleeping on your unaffected side can help keep your hips aligned and reduce pressure on the bursa. If you sleep on your back, a pillow under your knees may also help.
When should I see a doctor for hip pain?
Consider seeing a doctor if your hip pain is persistent, severe, interferes with your daily activities, or doesn’t improve after a week or two of self-care (rest, ice, over-the-counter pain relievers).