Subacromial bursitis is a painful inflammation of the bursa in your shoulder. It can limit your movement and make daily activities hard. In this post, find out what subacromial bursitis is, its symptoms, causes, and treatment options.
Key Takeaways
- Subacromial bursitis is an inflammation of the subacromial bursa, causing shoulder pain, especially during overhead movements.
- Diagnosis involves patient history, physical examinations, and imaging techniques like MRI, while treatment typically starts with conservative management including rest, medications, and physical therapy.
- Preventive measures such as ergonomic adjustments and regular exercise are essential for reducing the risk of bursitis and maintaining shoulder health.
What is Subacromial Bursitis?
Subacromial bursitis is an inflammation of the subacromial bursa, a small fluid-filled sac located beneath the acromion in the shoulder. This bursa acts as a cushion to reduce friction between the rotator cuff tendons and the overlying bony structures during shoulder movements. However, when the bursa becomes inflamed, it can result in significant shoulder pain and discomfort, potentially leading to subacromial impingement syndrome.
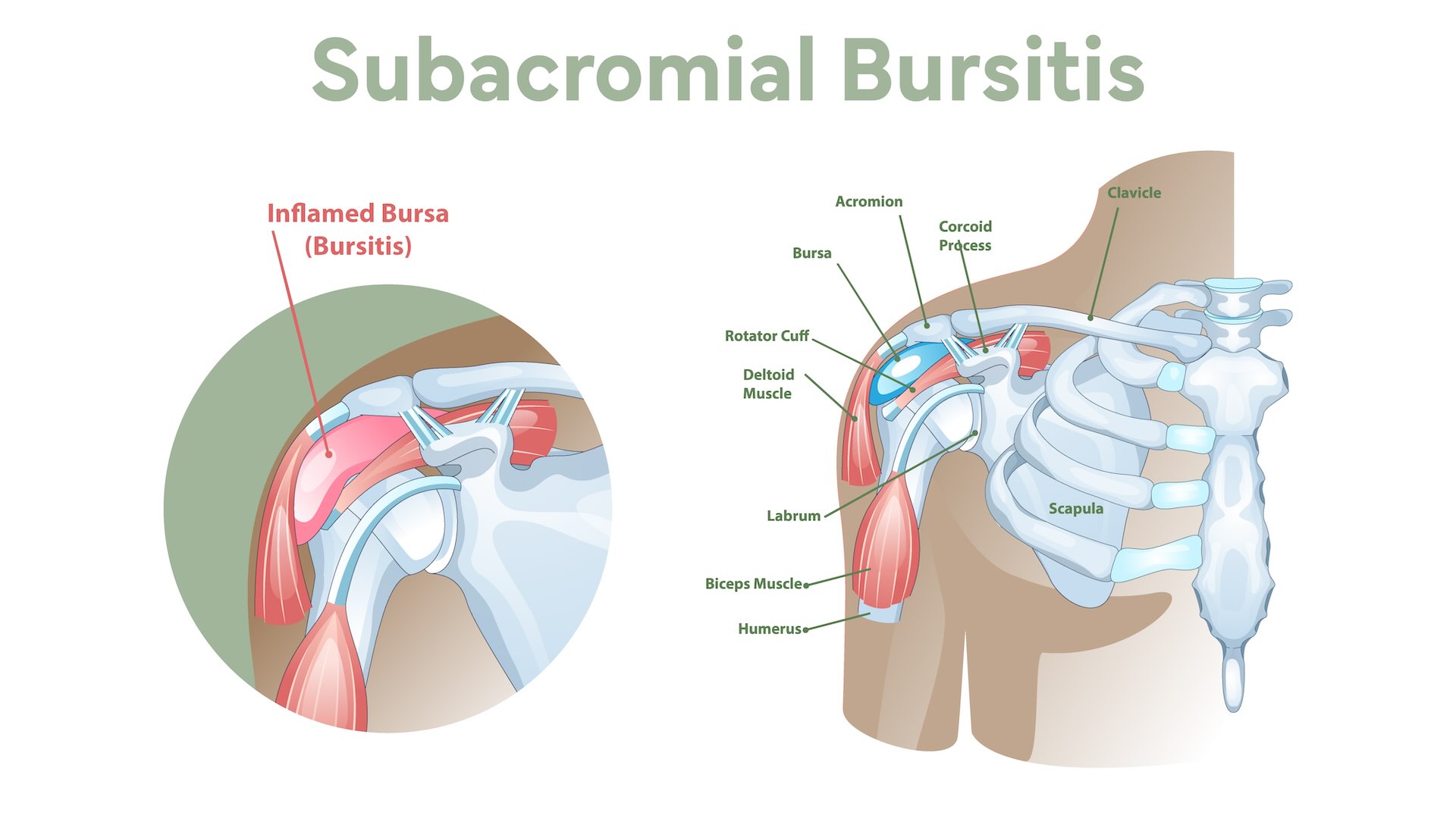
The inflammation leads to increased fluid and collagen production within the bursa, causing it to swell. This swelling results in the painful pinching of soft tissue, particularly when the arm is raised, as the space within the shoulder joint becomes constricted. The subacromial bursa is bordered by critical structures such as the acromion, coracoacromial ligament, and supraspinatus tendon muscle fibers. This proximity to vital components of the shoulder joint explains why inflammation can severely impact shoulder mobility and cause significant pain.
Clinical signs of subacromial bursitis typically include localized pain in the shoulder, which helps distinguish it from other shoulder issues. Recognizing this condition helps in identifying symptoms and seeking appropriate treatment, elaborated below.
Symptoms of Subacromial Bursitis
Before:
Early recognition of subacromial bursitis symptoms aids in diagnosis and management. Common symptoms consist of pain around the shoulder. There is also tenderness, particularly when raising the arm above the head. This pain is often described as a dull ache that is poorly localized, making it challenging to pinpoint the exact source.
After:
Common symptoms of subacromial bursitis include:
- Pain around the shoulder
- Tenderness, particularly when raising the arm above the head
- A dull ache that is poorly localized, making it challenging to pinpoint the exact source
Early recognition of these symptoms aids in diagnosis and management.
Tenderness and soreness are frequently felt along the front of the shoulder, particularly during overhead movements. The pain usually intensifies between 60° and 120° of arm elevation, a range known as the painful arc. This can significantly limit daily activities, such as reaching for objects on high shelves or performing overhead tasks.
In more advanced cases, the mobility of the shoulder may be severely restricted, impacting the ability to perform routine tasks. During a physical examination, pain may be elicited when resistance is applied beyond 75 to 80 degrees of arm abduction. These symptoms collectively highlight the need for timely and effective treatment to restore shoulder function and alleviate pain.
Causes and Risk Factors
Various causes and risk factors contribute to the development of subacromial bursitis. Individuals engaged in activities requiring repetitive overhead motions, such as athletes and manual laborers, are particularly prone to this condition. These repetitive movements can lead to microtrauma and inflammation of the subacromial bursa over time.
Before:
Direct trauma to the shoulder, such as falls or impacts, can also trigger inflammation. Age is another significant risk factor, as the likelihood of developing subacromial bursitis increases with the cumulative wear and tear on shoulder structures. Additionally, certain medical conditions, such as crystal deposition diseases, can contribute to the development of bursitis.
After:
Direct trauma to the shoulder can trigger inflammation. Key factors include:
- Falls or impacts
- Age, as the likelihood of developing subacromial bursitis increases with cumulative wear and tear on shoulder structures
- Certain medical conditions, such as crystal deposition diseases
Recognizing these risk factors aids in prevention and early intervention. By recognizing the activities and conditions that predispose individuals to subacromial bursitis, steps can be taken to mitigate these risks and maintain shoulder health.
Diagnosis of Subacromial Bursitis
Effective treatment relies on accurate diagnosis of subacromial bursitis. The process often begins with a thorough patient history, focusing on any trauma or repetitive overhead activities that could have led to shoulder pain. This initial step helps in distinguishing subacromial bursitis from other shoulder pathologies.
During the physical examination, point tenderness at the anterolateral aspect of the shoulder (the front and outer part) is a common finding. Provocative tests, where resistance is applied to the shoulder, may reveal weakness, indicating potential rotator cuff issues linked to the inflammation. These clinical signs are critical in forming a preliminary diagnosis.
When conservative treatments fail or there is uncertainty in the diagnosis, imaging techniques like MRI and ultrasound are employed. MRI, in particular, can assess bursal fluid accumulation and acromion morphology, providing a clearer picture of the inflammation. In some cases, arthroscopy may be performed to confirm the diagnosis if other methods are inconclusive.
Accurate diagnosis forms the cornerstone of effective treatment, detailed in the subsequent sections.
Treatment Options for Subacromial Bursitis
Treating subacromial bursitis involves a range of options, with non-surgical management being the primary approach. Most individuals see significant improvement with conservative treatments, which generally do not negatively impact daily life in the long term. However, in chronic or severe cases, surgical intervention may be necessary.
Let’s delve into these treatment options in detail.
Conservative Treatments
Conservative treatment for subacromial bursitis typically starts with rest and activity modification, allowing the shoulder to heal without further aggravation. Non-operative management also includes the use of oral NSAIDs for pain relief and corticosteroid injections to reduce inflammation. Repeated steroid injections, however, can cause infections and potential damage to the rotator cuff muscles.
Physical therapy is a cornerstone of conservative management, focusing on pain management strategies and therapeutic techniques like ice and heat therapy to alleviate pain and promote healing. Physical therapists also educate patients on exercises that strengthen the shoulder muscles and improve mobility, which are crucial for long-term recovery and preventing recurrences.
Adhering to a comprehensive conservative treatment plan allows most patients to find significant relief from bursitis symptoms and resume daily activities with minimal disruption.
Surgical Treatments
Surgical treatment is considered for patients with chronic bursitis that does not respond to conservative management or those with severe rotator cuff injuries. Surgical options include bursectomy, where the inflamed bursa is removed, and subacromial decompression, which involves removing part of the acromion to increase the space available for the rotator cuff tendons.
Rotator cuff repair may also be necessary in cases of severe rotator cuff tear or a rotator cuff injury. While surgery can provide significant relief, it is typically reserved for cases where other treatments have failed, ensuring that all less invasive options are exhausted first.
Preventing Subacromial Bursitis
A combination of strategies aimed at reducing shoulder strain can prevent subacromial bursitis. Ergonomic adjustments, such as aligning your computer screen at eye level, can help minimize shoulder strain and prevent the condition. Regular shoulder movements and exercises strengthen the shoulder and increase its resilience to pain.
For individuals involved in repetitive overhead activities, long-term management and preventive measures are crucial to avoid recurrences. This can include modifying activities to reduce overhead motions and incorporating regular breaks to give the shoulder time to recover.
Adopting these preventive strategies greatly reduces the risk of developing subacromial bursitis and supports healthy shoulder function.
Prognosis and Long-term Management
The prognosis for subacromial bursitis is generally good, as it is a self-limiting condition that often resolves on its own. With appropriate conservative treatment, many patients experience significant improvement. However, outcomes can be poorer for older patients due to the cumulative wear and tear on shoulder structures.
Long-term management involves maintaining a healthy lifestyle, which includes stress management techniques like meditation to positively influence pain perception and ensuring adequate sleep to aid overall recovery. An anti-inflammatory diet consisting of whole foods can also help reduce joint pain associated with bursitis.
Effective management of shoulder stiffness and pain prevents disruptions in daily life and ensures a smooth recovery process. Chronic bursitis can develop as a complication, leading to persistent shoulder pain and mobility issues, hence the need for ongoing management strategies.
Complications of Subacromial Bursitis
If subacromial bursitis is not addressed in a timely manner, it can lead to several complications. Chronic bursitis can result in sustained pain and weakness, potentially causing damage to the tendons. While there is no significant difference in the incidence of rotator cuff tears related to the number of steroid injections, repeated injections do carry risks.
These risks include infections and potential damage to the rotator cuff muscles, highlighting the importance of cautious use of steroid injections. Increased friction due to ongoing shoulder activities can exacerbate the condition and lead to further complications. Timely and effective treatment prevents these issues and maintains shoulder health.
Enhancing Recovery Through Physical Therapy
Physical therapy is crucial in the recovery process for subacromial bursitis. It focuses on enhancing muscle strength and improving mobility, which are key to preventing future shoulder injuries. By incorporating targeted exercises, physical therapy helps strengthen the shoulder muscles and increase the range of motion.
Stretching exercises are commonly utilized to regain range of motion and flexibility in the shoulder. Physical therapists also employ hands-on therapy techniques to restore mobility and relieve tension in the shoulder.
These comprehensive physical therapy strategies are vital for achieving long-term pain relief and preventing recurrences of subacromial bursitis.
Summary
In summary, subacromial bursitis is a common cause of shoulder pain that can significantly impact daily activities. Understanding its symptoms, causes, and treatment options is crucial for effective management. Conservative treatments, including physical therapy, play a vital role in recovery, while surgical options are reserved for more severe cases. Preventive measures and long-term management strategies are essential to maintain shoulder health and prevent recurrences. With proper care and attention, individuals can manage subacromial bursitis effectively and enjoy a pain-free life.
Frequently Asked Questions
What is subacromial bursitis?
Subacromial bursitis is the inflammation of the subacromial bursa, which plays a crucial role in reducing friction in the shoulder during movement. This condition can lead to pain and limited mobility in the affected shoulder.
What are the common symptoms of subacromial bursitis?
The common symptoms of subacromial bursitis are shoulder pain, tenderness, and reduced mobility, especially when lifting the arm overhead. These signs indicate that you may need to seek further evaluation or treatment.
How is subacromial bursitis diagnosed?
Subacromial bursitis is diagnosed through a combination of patient history, physical examination, and imaging techniques such as MRI or ultrasound. This comprehensive approach ensures accurate identification of inflammation in the area.
What are the treatment options for subacromial bursitis?
The primary treatment options for subacromial bursitis include conservative methods such as rest, NSAIDs, corticosteroid injections, and physical therapy, with surgery considered for chronic or severe cases. These approaches aim to reduce inflammation and improve shoulder function effectively.
How can subacromial bursitis be prevented?
To prevent subacromial bursitis, focus on ergonomic adjustments, incorporate strengthening exercises, and modify activities to alleviate shoulder strain. Implementing these strategies can significantly reduce the risk of developing this condition.