The shoulder joint offers the widest range of motion of any joint in the human body. This mobility, however, comes at a cost: a predisposition to instability. Shoulder instability occurs when the structures that hold the ball of the upper arm bone (humerus) securely within the shallow socket of the shoulder blade (glenoid) are compromised. In this post, we’ll explore shoulder instability, covering its causes, symptoms, various treatment options, expected recovery times, and prevention strategies.
Key Takeaways
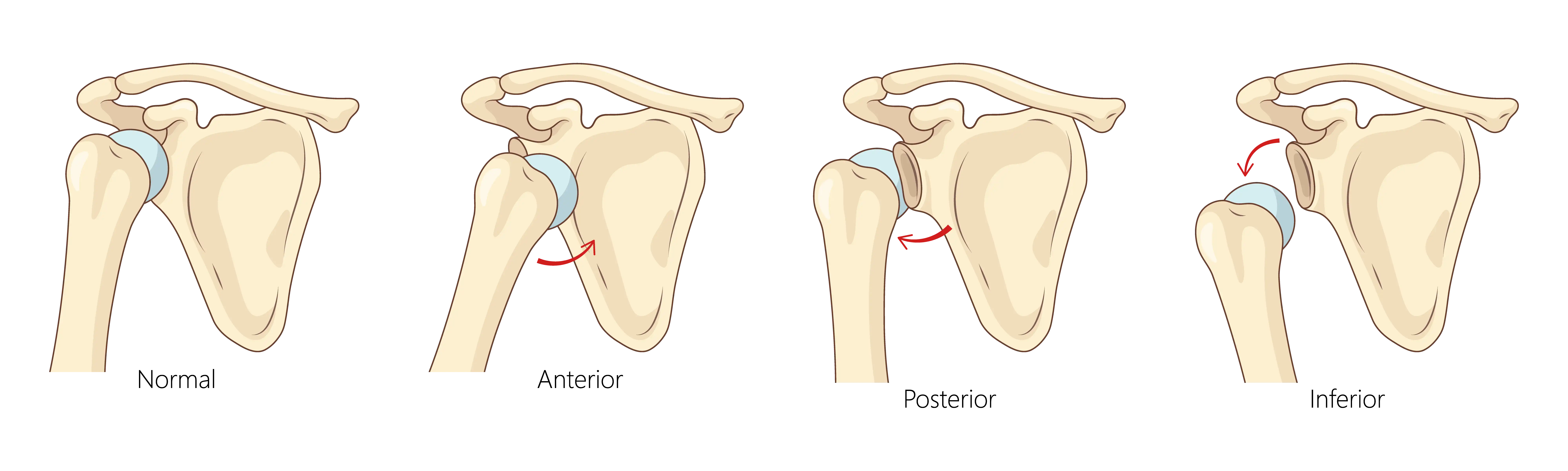
- Shoulder instability occurs when the head of the upper arm bone (humerus) is no longer firmly centered in the shoulder socket (glenoid). This can range from a feeling of looseness to a complete dislocation.
- It often results from traumatic injuries like falls or sports accidents, but can also stem from repetitive overhead motions.
- Treatment options range from conservative methods like physical therapy and activity modification to surgical interventions, depending on the severity and underlying cause.
What is Shoulder Instability?
The shoulder joint is a ball-and-socket joint, but unlike the hip, the socket is shallow, resembling a golf ball on a tee. Stability is primarily provided by a complex interplay of stabilizers, including the labrum, joint capsule, and rotator cuff muscles. When any of these stabilizers are damaged or weakened, the shoulder can become unstable.
Causes of Shoulder Instability
Shoulder instability can arise from a variety of factors, including acute trauma, repetitive stress, and genetic predisposition. The underlying cause influences recommended treatment strategies.
Traumatic Injury
Traumatic injury is a common cause of shoulder instability. A significant force can push the humeral head out of the glenoid socket, leading to damage to the surrounding structures. Common scenarios include:
- Falls: Landing directly on the shoulder or on an outstretched arm.
- Sports Injuries: High-impact sports like football, rugby, hockey, or sports involving overhead movements, where direct blows or sudden, forceful movements can dislocate the shoulder.
- Motor Vehicle Accidents: Direct trauma to the shoulder during a collision.
Atraumatic Instability
Unlike traumatic instability, atraumatic instability develops gradually, often without a specific injury event. This type of instability can be influenced by:
- Repetitive Microtrauma: Overhead athletes (e.g., swimmers, baseball pitchers, tennis players) who perform repetitive motions can gradually stretch the joint capsule and ligaments over time, leading to increased laxity and instability.
- Muscle Imbalance/Poor Neuromuscular Control: Weakness or imbalance in the rotator cuff and scapular stabilizing muscles may lead to improper mechanics and increased stress, eventually causing instability.
Other Contributing Factors
- Genetic Predisposition: Some individuals may have a genetic predisposition to looser ligaments or weaker connective tissues, making them more susceptible to instability.
- Previous Shoulder Injuries: A history of shoulder dislocation or subluxation may increase the risk of future episodes. Each episode can further stretch or damage the stabilizing structures.
Understanding the potential causes of shoulder instability is helpful for effective treatment planning.
Symptoms of Shoulder Instability
The symptoms of shoulder instability can vary widely. They can range from subtle sensations of looseness to debilitating pain following a complete dislocation. Recognizing these symptoms supports early diagnosis and intervention.
One potential symptom is recurrent dislocations or subluxations. A dislocation is when the humeral head completely comes out of the socket. A subluxation is a partial dislocation where the humeral head partially slips out and then spontaneously reduces (goes back in).
Pain is another common symptom, which can be acute and severe during a dislocation or subluxation, or a dull, persistent ache in chronic cases. Pain may worsen with certain movements, especially overhead activities or reaching across the body. Additionally, patients may report a feeling of looseness, weakness, numbness, or crepitus (clicking, popping, or grinding sensations).
Diagnosis of Shoulder Instability
An accurate diagnosis is important for developing an effective treatment plan. This typically involves a detailed medical history, a comprehensive physical examination, and often, imaging studies.
Your doctor will typically begin by asking questions about your symptoms and medical history, including when the symptoms began, previous injuries, and family history. A comprehensive physical examination of both shoulders may be performed to assess range of motion and strength.
Imaging studies are often used to confirm the diagnosis, identify associated injuries, and plan for treatment. X-rays are typically the first imaging study performed to help with confirming a dislocation, identifying any fractures, and assessing the alignment of the joint. Magnetic resonance imaging (MRI) may be used to provide detailed images of the soft tissues.
Treatment Options for Shoulder Instability
Treatment for shoulder instability is tailored to the individual patient, taking into account the type and severity of instability, the patient’s age, activity level, and associated injuries. The primary goal is to restore stability, relieve pain, and return the patient to their desired level of function. Treatment can be broadly categorized into non-surgical and surgical options.
Non-Surgical Treatment
Non-surgical treatment is often the first line of defense. Options may include:
- Activity Modification: Avoiding activities and arm positions that trigger instability may be a key first step. This may involve modifying work tasks, sports techniques, or daily habits.
- Pain and Inflammation Control: Rest, ice, and nonsteroidal anti-inflammatory drugs (NSAIDs) can help manage pain and swelling.
- Physical Therapy: This is the cornerstone of non-surgical treatment. A structured physical therapy program may focus on:
- Strengthening the Rotator Cuff and Scapular Stabilizers: A targeted exercise program to improve the strength and endurance of the muscles that dynamically stabilize the shoulder.
- Neuromuscular Re-education: Training the muscles to fire in the correct sequence to maintain joint stability during movement.
- Proprioceptive Training: Improving the joint’s sense of position to enhance stability.
- Core Strengthening: A strong core provides a stable base for all arm movements.
Surgical Treatment
Surgery is often recommended for patients with recurrent instability, especially young athletes, or for those who have failed to improve with non-surgical treatment. While the specific surgical procedure depends on the cause of the instability, the overall goal of surgery is to repair the damaged structures. Many of these procedures can be performed arthroscopically, using small incisions and a tiny camera, which minimizes scarring and can lead to a faster recovery.
An experienced orthopedic surgeon can evaluate the condition and help recommend the best treatment option for you.
Recovery Time
Recovery from shoulder instability treatment can vary depending on the type of treatment (non-surgical vs. surgical), the specific surgical procedure performed, and individual patient factors. Patience and adherence to the rehabilitation protocol are key to a successful outcome.
Non-Surgical Recovery
For patients undergoing non-surgical treatment, improvement is often gradual. It may take several months of dedicated physical therapy to achieve improvement in strength, stability, and function.
Surgical Recovery
Recovery after surgery is more structured and typically follows a phased protocol:
- Immobilization: After surgery, the arm is often placed in a sling to protect the repair. During this time, gentle passive range of motion exercises may be initiated to prevent stiffness.
- Active Range of Motion: Once the initial healing has occurred, the sling may be gradually discontinued, and the patient begins active range of motion exercises to restore mobility.
- Strengthening: A progressive strengthening program is initiated.
- Return to Sport/Activity: For athletes, a sport-specific training program is started to prepare for a safe return to competition.
While recovery times vary depending on the individual, return to full activity generally takes anywhere from 6 months to a year. It is essential to follow the guidance of your orthopedic surgeon and physical therapist to avoid re-injury and ensure the best possible outcome.
Prevention Strategies
While it may not be possible to prevent all traumatic dislocations, there are several strategies that can help reduce the risk of shoulder instability:
- Strengthening Programs: A regular exercise program focused on strengthening the rotator cuff and scapular stabilizing muscles can support shoulder stability.
- Proper Technique: In sports, proper technique and biomechanics can reduce stress on the shoulder joint.
- Warm-up and Cool-down: Warm up properly before exercise and cool down afterwards to prepare the muscles for activity.
- Avoid Risky Behaviors: Be mindful of activities that put you at high risk for falls or collisions.
- Protective Gear: In contact sports, wearing appropriate protective gear can help prevent injuries.
- Listen to Your Body: If you experience shoulder pain or fatigue, don’t push through it. Rest and seek medical advice if necessary.
Summary
Shoulder instability is a complex condition that can impact an individual’s quality of life. However, with a thorough understanding of the underlying causes, a comprehensive diagnosis, and a tailored treatment plan, for many patients, it can be possible to restore stability, relieve pain, and return to the activities you love. Whether through a dedicated physical therapy program or a surgical procedure, the goal is to help restore function. If you are experiencing symptoms of shoulder instability, consider seeking expert orthopedic care.
Frequently Asked Questions (FAQ)
Can a dislocated shoulder heal on its own?
While the immediate pain of a dislocation may subside after the shoulder is reduced (put back in place), the underlying damage to the labrum, ligaments, and capsule may not heal on its own. This is why recurrent instability is more common after a first-time dislocation. If experiencing shoulder instability, consider seeking medical evaluation.
Is surgery always necessary for shoulder instability?
No, surgery is not always necessary. For some injuries, non-surgical treatment may be an option. However, for certain individuals, especially those with recurrent traumatic instability, surgery may be recommended to prevent further episodes and long-term damage to the joint.
What’s the difference between subluxation and dislocation?
A subluxation means the ball of the shoulder briefly slips out of place but goes back on its own. A dislocation means it comes all the way out and usually needs medical assistance to be reduced back into place.